Adrian Boucher, R.Ph, B.Sc, PharmD 1,2
Larry Sheng, B.Sc, PharmD Student2,3
Certina Ho, R.Ph, B.Sc.Phm, MISt, M.Ed, PhD 1,2,3
1 Leslie Dan Faculty of Pharmacy, University of Toronto
2 Institute for Safe Medication Practices Canada
3 School of Pharmacy, University of Waterloo
Given the complexity of the pharmacy workflow, medication incidents are an inevitable part of practice. In fact, it is estimated that as many as seven million medication incidents could occur in Canadian community pharmacies in a year.1 Reporting, analyzing, and learning from medication incidents are key components of the College’s Medication Safety Program or any other continuous quality improvement (CQI) program that aims to reduce the risk of future recurrences. Unfortunately, reporting and discussion of incidents in pharmacies is a responsibility that is often avoided, due to fear of potential retribution from both fellow colleagues and management.1
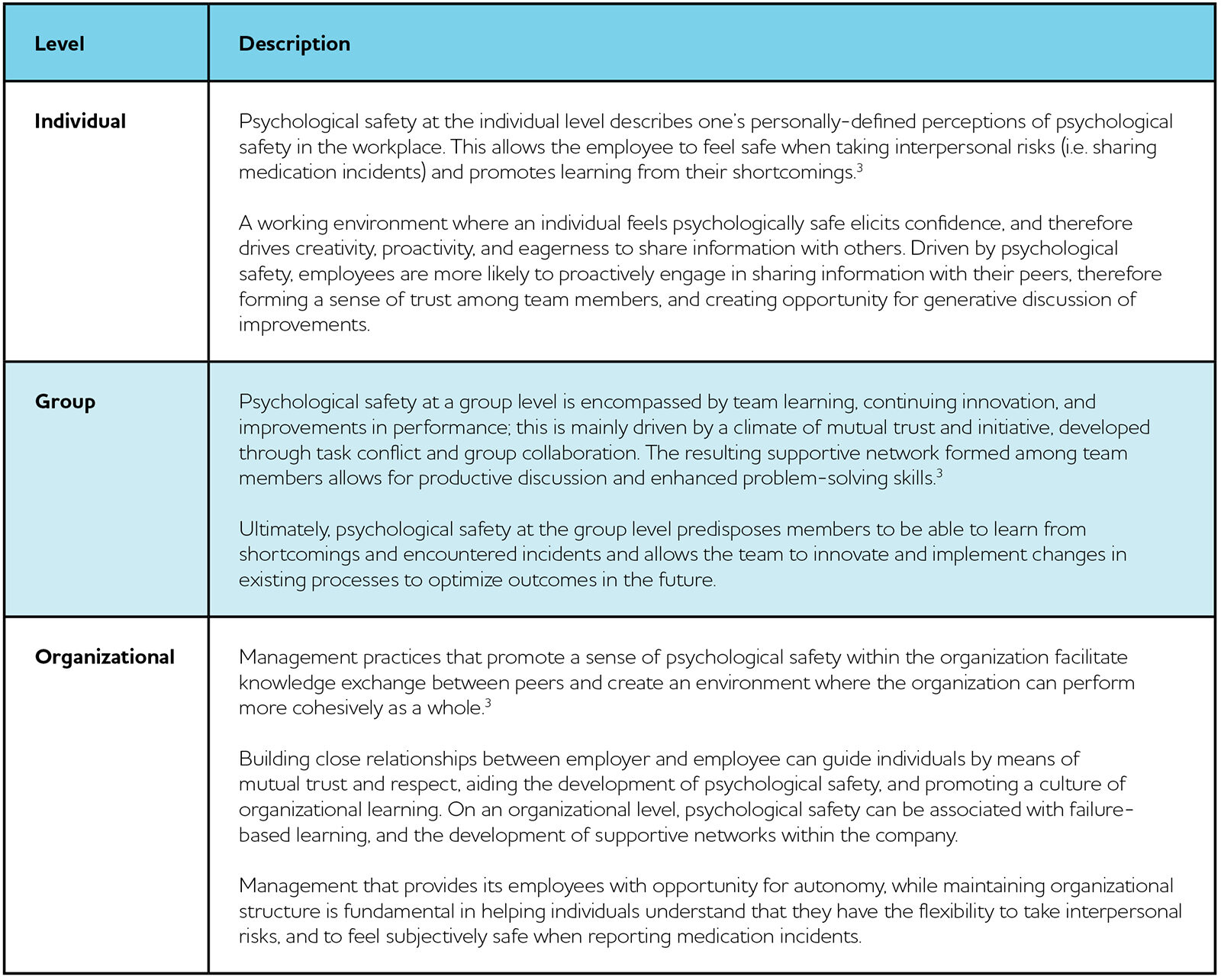
Overcoming these barriers is necessary to create an environment of psychological safety. Psychological safety refers to the phenomenon where members of a team are comfortable with taking interpersonal risks, such as reporting and discussing medication errors, without fear of negative consequences to self-image, status, or career.2 In healthcare, where errors form the basis upon which improvements in processes are established, psychological safety sets the foundation in allowing both organizations as well as individual practitioners to learn from not only their own, but also from their colleagues’ errors. The effects of psychological safety can be expressed across three different levels: individual, group, and organizational (Table 1).
Table 1. Effect of Psychological Safety at the Individual, Group, and Organizational Levels
CREATING AN ENVIRONMENT OF PSYCHOLOGICAL SAFETY
Development of psychological safety within the workplace allows for understanding of organizational learning and promotes sharing of errors via upwards communication. This encourages staff to express concerns and share incidents not only among their peers, but also with executive staff members, resulting in potential for implementation of organization-wide changes and improvements.3
To develop a work culture that embraces psychological safety, factors that influence employees’ subjective perception of the work environment must first be established. These include promotion of interpersonal relationships, management behaviours, and organizational practices that are present in the workplace. Cumulatively, these factors should aim to drive the continuous development of psychological safety and ensure that employees consistently feel comfortable with sharing any incidents that they encounter.
Interpersonal Relationships
Interpersonal relationships, and the social support and resources inherent within, promote psychological safety and contribute to team learning, performance, and innovation.4 Growth of interpersonal relationships is essential in encouraging team collaboration, and the support of peers willing to provide constructive feedback is often a primary objective in helping employees establish a sense of belonging within a team. When relationships among the team are supportive and trusting, members are given the opportunity to manage interpersonal risks and proactively report incidents without fear of repercussions.3
Management Behaviours
Supportive and clarifying management processes are the most effective management styles in promoting psychological safety in the workplace.3 Management characteristics such as inclusiveness, support, trustworthiness, openness, and behavioral integrity strongly influence employee perceptions of psychological safety, which in turn, fosters beneficial outcomes such as team learning behavior, team performance, engagement in quality improvement work, and reduction in errors amongst team members.4
Organizational Practices
Supportive organizational practices are positively related to employee work outcomes such as organizational commitment and job performance as they heighten perceptions of psychological safety.4 The intimacy of a smaller, enclosed system effectively promotes open discussion and increased willingness of staff to express concerns and share incidents.3
PSYCHOLOGICAL SAFETY AND CONTINUOUS QUALITY IMPROVEMENT (CQI)
The recent implementation of the College’s Medication Safety Program highlights the importance of psychological safety. The Medication Safety Program requires community pharmacies to conduct proactive reviews of existing work processes to identify areas of risk and retrospective reviews of medication incidents to help prevent recurrences in order to enhance medication safety. The incident reports generated will not only help individual pharmacies to develop quality improvement initiatives, but also allow aggregate analysis to inform the development of resources to address gaps in knowledge and skills, and support shared learning across Ontario.5
Psychological safety will be necessary to creating a culture where individuals are comfortable bringing forward medication incidents without fear of punitive outcomes. This aligns with the principles of a just culture upon which the College’s Medication Safety Program is built.5 Without psychological safety, pharmacy staff will be less likely to report errors, suggest new ideas, or seek assistance. Training of pharmacy staff, support from upper management, and frequent follow-up or monitoring from pharmacy regulatory authorities will be necessary to create this environment. By focusing on reducing barriers to achieving psychological safety, pharmacies can create a more open work environment and improve overall patient safety.
REFERENCES
1. Boyle TA, Mahaffey T, MacKinnon NJ, Deal H, Hallstrom LK, Morgan H. Determinants of medication incident reporting, recovery, and learning in community pharmacies: a conceptual modetl. Res Social Adm Pharm 2011 Mar; 7(1): 93-107.
2. Edmondson AC, Lei Z. Psychological safety: The history, renaissance, and future of an interpersonal construct. Annu Rev Organ Psychol Organ Behav 2014; 1: 23-43.
3. England I, Stewart D, Walker S. Information technology adoption in health care: when organisations and technology collide. Aust Health Rev 2000; 23(3): 176-85.
4. Newman A, Donohue R, Eva N. Psychological safety: A systematic review of the literature. Human Resource Management Review 2017; 27(3): 521-535.
5. Ontario College of Pharmacists (OCP). Preparing for Ontario’s Medication Safety Program. Pharmacy Connection 2018; Spring: 17-20.