As part of the College’s continuing commitment to its Opioid Strategy, the College recently released the Opioid Dispensing in Ontario: 2018 Snapshot. The snapshot, which is available on our website, is intended to provide an overall look at opioid dispensing patterns in Ontario related to three areas of analysis that are considered high-risk dispensing practices. In publishing the snapshot, the College is seeking to better understand practice behaviours, with the primary goal of identifying areas for further teaching, coaching and collaborating with pharmacy professionals in preventing opioid-related harms.
The College also recognizes that there is growing public, patient and health system stakeholder interest in understanding the role of pharmacy in helping to reduce the human and societal impact associated with the opioid crisis in our communities. Publicly reporting this information can help guide quality pharmacy care and do so openly and transparently so that the entire health system can better understand these patterns and contribute as appropriate to quality improvement activities.
Of equal importance is providing pharmacy professionals with information to help them evaluate and enhance their own practice as medication experts. Pharmacy professionals are strongly encouraged to assess their own dispensing practices, using the provincial data provided and any other data they have access to (i.e. trends identified regionally, tracking in their organization) to look for opportunities to enhance the patient care they are providing. In the snapshot, the College has provided a number of key considerations for pharmacy professionals who are dispensing opioids.

A PICTURE OF OPIOID DISPENSING
The data analysis in the snapshot was provided by the Ministry of Health from the Narcotics Monitoring System (NMS). The Ministry is responsible for the management of the NMS and conducted the analysis before sharing the aggregate, de-identified data analysis with the College. The data analysis did not identify specific pharmacies, pharmacy professionals or patients.
The data analysis is focused on three areas of opioid dispensing:
- incidence of high-dose opioid prescriptions (i.e. new prescriptions for patients who did not receive an opioid in the previous six months);
- prevalence of high-dose opioid prescriptions; and
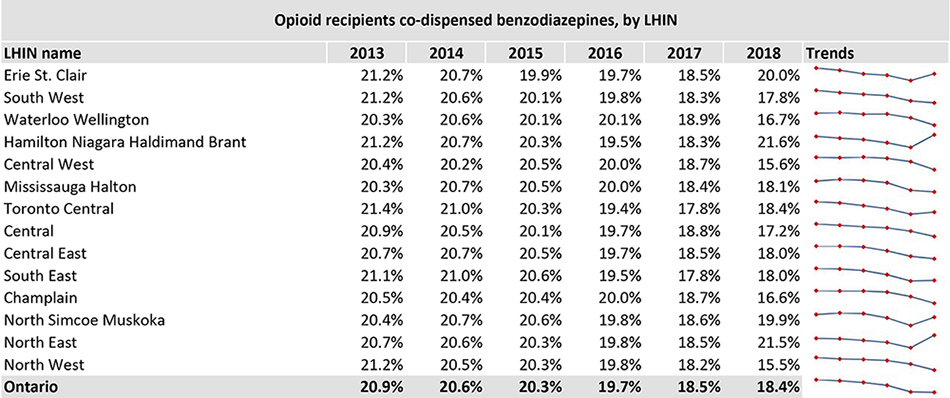
- opioid and benzodiazepine co-dispensing.
For the purposes of organizing the data and recognizing that there will be variations among regions, the data analysis is provided by Local Health Integration Network (LHIN)* as well as provincially.
It’s important to note that the data analysis for a specific LHIN does not represent a benchmark or standard for pharmacy practice. Rather, the value of the data analysis is in providing a way to measure the impact of shifts in pharmacy practice over time and place and identify opportunities for improvement. The key considerations highlighted in the snapshot provide initial areas of focus for pharmacy professionals who are exploring where there is an opportunity to contribute to enhanced patient and system outcomes.
The College also recognizes that while this snapshot focuses on the opportunities for pharmacy professionals to enhance their practice, the dispensing of opioids also involves other healthcare professionals and various system factors. Accordingly, the College continues to look for opportunities for conversation and collaboration with the many organizations and healthcare professionals who are also committed to preventing patients from experiencing opioid-related harms. For more information on why the College released the opioid dispensing snapshot, please review the Frequently Asked Questions on the Opioid Dispensing in Ontario Snapshot on the OCP website.
Example table from the Opioid Dispensing in Ontario Snapshot
KEY CONSIDERATIONS FOR PHARMACY PROFESSIONALS
The snapshot provides an opportunity for pharmacy professionals to assess and evaluate their own opioid dispensing practice. The College has highlighted a few key considerations when doing so in both the snapshot and the one-page Resource for Pharmacy Professionals.
The considerations particularly focus on patient assessment and education. It is important to assess whether the prescribed opioid therapy is appropriate for the patient, including, but not limited to, their conditions, history, characteristics of their pain, possible treatment alternatives, possible risks to the patient and monitoring parameters, such as adverse effects. Complete documentation of this assessment should be readily accessible for continuity of care.
The snapshot chiefly focuses on high-dose opioid prescriptions since high doses of opioids, where a low dose may suffice, are associated with increased risk of adverse events including emergency department visits or hospitalizations, substance use disorder, and even overdose deaths.[1] Pharmacists should assess each opioid prescription to ensure that it is started at the lowest dosage necessary for that patient. This may involve collaboration with the prescriber and the suggestion of alternative medication and dosages.
One of the areas of data analysis is the co-dispensing of opioids and benzodiazepines, which despite numerous guidelines contraindicating concurrent use of opioids and benzodiazepines, are often co-prescribed[2]. Pharmacists are expected to assess situations within which opioid and benzodiazepines are co-prescribed, and examine the rationale for their concurrent use. Collaboration with patients and prescribers is critical to ensure potential adverse events, such as respiratory depression, are identified and prevented where possible.
Finally, it is important that appropriate education is provided to patients regarding their opioid prescription. For example, if the opioid prescribed is indicated for acute pain, patients should also be provided information on the characteristics of acute pain, including its self-limiting nature, and expected duration.
The College provides a number of resources to help pharmacy professionals identify and implement best practices with regards to dispensing opioid prescriptions, including:
- the Opioid Practice Tool;
- the Opioid Policy;
- and External Resources on Opioids.
NEXT STEPS
Ultimately, the goal of the snapshot is to identify opportunities, through greater awareness of patterns made possible through analyzed data, to influence quality improvement and safe pharmacy practice and enhance system and patient outcomes.
The College anticipates that it will provide updated data for the most recent year on an annual basis. Over time, the data analysis will provide an overview of the impact of the various activities and strategies being undertaken by pharmacy, and the larger healthcare system, on opioid dispensing. It is anticipated that greater awareness of the data and opioid dispensing trends by pharmacy professionals will lead to improved practice and better patient health outcomes.
The College will also continue to look for opportunities to provide learnings and resources for pharmacy professionals that reflect the findings/needs identified through the data analysis. Feedback from pharmacy professionals, stakeholders and patients will also be taken into account when looking at future reporting opportunities.
*Throughout the data analysis, the term LHIN is used to describe specific regions. At the time of the data analysis, Local Health Integration Networks were geographically based organizations that plan, integrate and fund local health care. However, future reporting formats are subject to change as the structure of the provincial health system transforms and evolves over time.
- https://www.sciencedirect.com/science/article/pii/S0197457218302015 ?
- https://www.sciencedirect.com/science/article/pii/S0197457218302015 ?













