By Ian Stewart R.Ph, B.Sc.Phm.
Failure to accurately process information is a human factor which often results in the occurrence of medication errors. Confirmation bias is often a contributing factor.
Confirmation bias is the tendency of people to look for and interpret information in a way that confirms their beliefs or hypotheses and to ignore or not look for information which is contradictory. We therefore tend to see’ what is in our memory or what we believe to be true.
The similarity of drug names together with confirmation bias can lead to a medication error as the following case demonstrates.
CASE:
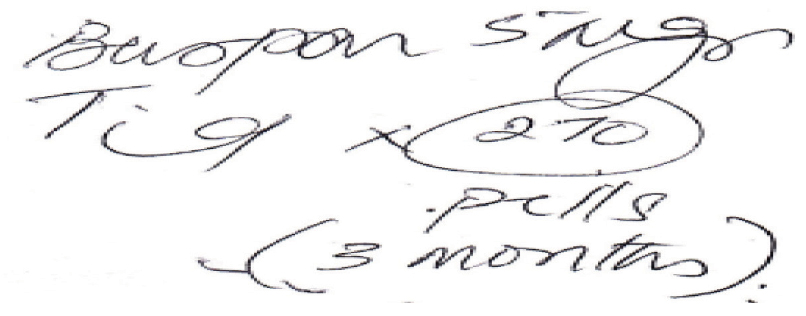
The above prescription was presented to a pharmacy assistant at a community pharmacy. The prescription was interpreted and entered as Buscopan® tablets with the instructions to take half a tablet three times daily. The Buscopan® tablets were therefore prepared and given to the pharmacist for checking.
Upon checking the prescription, the pharmacist identified that the physician prescribed Buspar® and not Buscopan®. The change was therefore made and the patient received the correct medication.
POSSIBLE CONTRIBUTING FACTORS:
- Buspar® and Buscopan® can look similar when written.
- The pharmacy assistant was unfamiliar with the drug Buspar® and therefore did not consider it as a possibility. On the other hand, Buscopan® was often dispensed. As a result, the pharmacy assistant likely saw what was familiar.
- The patient’s medication history was not consulted by the pharmacy assistant entering the prescription to identify any similarity or changes in drug therapy.
RECOMMENDATIONS:
- Be aware of the potential for confirmation bias when dispensing drugs with similar names. Educate all pharmacy staff about problematic drug pairs that may be misinterpreted.
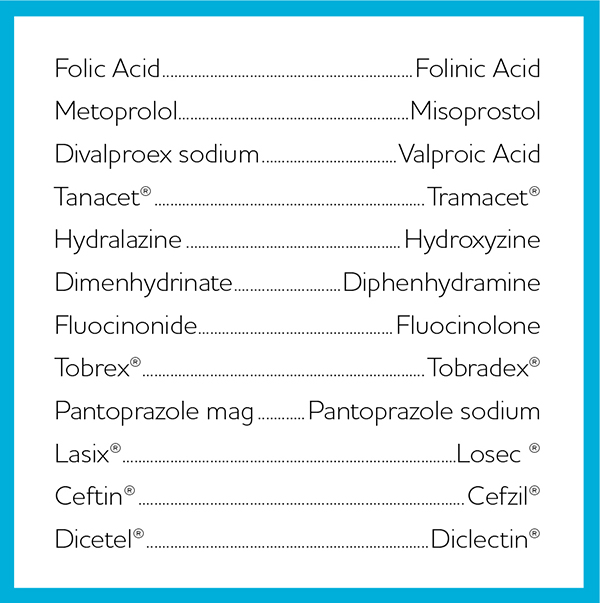
Below is an abbreviated list of problematic drug pairs. A more comprehensive list can be accessed at: http://www.ismp.org/tools/confuseddrugnames.pdf.
- The patient’s medication history should be consulted to identify changes in drug therapy or potential prescribing errors.
- When counselling the patient, ask open ended questions including, What did the doctor tell you this medication is for? Also, What did he/she tell you to expect from this medication?
- When dispensing a specific drug, consider all aspects of the prescription for appropriateness. Factors to be considered include the patient parameters, medication history, indication for use, the dose, dosing interval, duration of therapy, etc.
Please continue to send reports of medication errors in confidence to Ian Stewart at: ian.stewart2@rogers.com. Please ensure that all identifying information (e.g. patient name, pharmacy name, healthcare provider name, etc.) are removed before submitting.













