This article originally appeared in the Spring 2017 issue of Pharmacy Connection.
Ethical issues and dilemmas are a reality of everyday practice. The ability to make sound ethical decisions is a fundamental responsibility of pharmacists and pharmacy technicians as healthcare professionals.
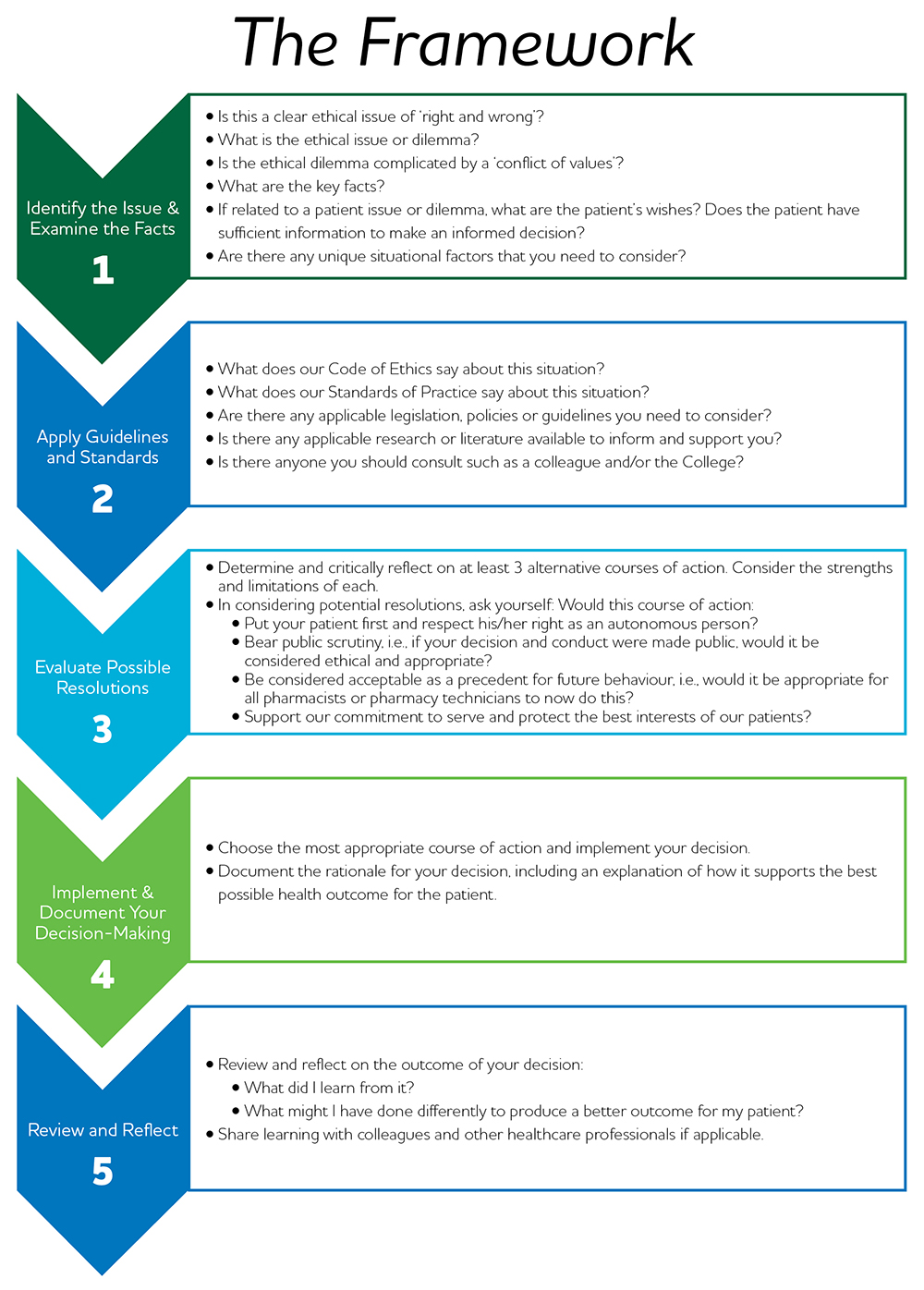
Designed to enhance objectivity and consistency, the Framework for Ethical Decision-Making provides a systematic thought-provoking process to guide decision-making and document decisions made in practice that support our commitment to serve and protect our patients’ best interests.
When confronted with an ethical issue or dilemma, pharmacists and pharmacy technicians should systematically work through the steps outlined in the Framework.
Ethical Decision-Making
IN PRACTICE
AN EXAMPLE OF AN ETHICAL DILEMMA
After the narcotic order is received and reconciled at a community pharmacy, the pharmacist asks the pharmacy technician who is working that day to put away the order because the technician who usually manages the order is away sick. As the pharmacy technician is putting away the checked order, she looks at the previous orders for the month. She notices that quite a few of the previous orders include OxyNEO®, which she does not recall seeing in the pharmacy stock. On the previous order she notes that four bottles of OxyNEO® 20 mg were ordered. However, she recently had a patient with a prescription for that strength and the pharmacy didn’t have any in stock and the patient ended up taking his prescription to another pharmacy. The only staff employed by the pharmacy are herself, the other technician and the owner. She suspects that the other pharmacy technician is diverting the OxyNEO®.
When presented with any ethical issue, pharmacy professionals should consider and apply the ethical principles of healthcare to determine the most appropriate ethical decision. If you are presented with a more complex situation, such as the one above involving a personal conflict of interest, it may be beneficial to take a more structured approach to decision-making to ensure that only the established ethical principles of healthcare, not your own personal values or beliefs, guide your decision-making.
The Ethical Decision-Making Framework can be used to assist pharmacy professionals in assessing a situation that poses a more complex ethical dilemma.
1. IDENTIFY THE ISSUE AND EXAMINE THE FACTS
The first step in assessing a complex ethical dilemma is to identify the key ethical issue(s) and then the facts of the situation. It is important to keep in mind that the facts surrounding the ethical issue include information that is known to exist or to have happened and are not influenced by the ethical issue itself.
In the above case, the pharmacy technician has noted that a quantity of narcotic drugs (OxyNEO®) is unaccounted for in the pharmacy. Of the three people on staff at the pharmacy, only one pharmacy technician routinely manages drug orders for the pharmacy. The pharmacy technician that has identified the discrepancy has strong evidence that the other pharmacy technician on staff has engaged in unethical behaviour.
If the pharmacy technician suspects that her colleague is diverting narcotic drugs, she has an ethical duty to report this to the Designated Manager for further investigation. There is also a professional duty of the pharmacy technician to report unethical behaviour by colleagues to the appropriate regulatory authority.
If an issue is identified in a pharmacy, simply reporting the employee within the organization or terminating employment is not enough. As a healthcare professional, you have a duty to act in society’s best interest. If a Designated Manager releases an individual from employment and the individual is not reported (by either yourself or the Designated Manager) to the appropriate regulatory body, you could be putting patients at other pharmacies and the public at risk if this former employee is simply hired at another pharmacy.
2. APPLY GUIDELINES AND STANDARDS
The Ethical Principles and Standards in the Code of Ethics provide guidance on expectations of conduct and behaviour. Standards of Practice set out minimal expectations of practice and provide guidance about the knowledge, skills, judgment and attitudes that members should apply to their practice to provide patients with safe and ethical care. College policies, guidelines and other supporting resources provide additional clarification on certain areas of practice. Legislation and regulations set out rules or requirements for the operation of a pharmacy and for individual practice. All of these can be applied when considering an ethical dilemma.
In this case example, pharmacy professionals are required to keep records of narcotic purchases and losses in accordance with relevant policies, guidelines and legislation. The Standards of Practice, legislation and College policies also outline requirements for narcotic inventory management. Review of the processes and narcotic records in the pharmacy against the requirements outlined in relevant resources would provide information indicating whether appropriate narcotic management is occurring in the pharmacy.
Examples of resources that should be considered with this case are:
- Code of Ethics Standards under Principle of Accountability
- Standards of Practice for Pharmacy Technicians Standards under Standard 1: Expertise in drug distribution systems and Standard 4: Professionalism and Ethics
- Narcotic Control Regulations under the Controlled Drugs and Substances Act
- Medication Procurement and Inventory Management Policy
- Resources under the Narcotics Practice Tool that include Fact Sheets on Narcotic Purchases, Narcotic Purchase Records, Narcotic Reconciliation and Security and Narcotic Reporting of Loss
- The Code of Ethics section of the website provides an overview of the various resources related to the core principles that dictate a healthcare professional’s ethical duty to patients and society.
Related Standard: 4.10
Members report professional incompetence or unethical behaviour by colleagues or other healthcare professionals to the appropriate regulatory authority.
3. EVALUATE POSSIBLE RESOLUTIONS
The resources identified, including relevant ethical standards, should be used to determine possible resolutions to an ethical dilemma. Here are three options for this case, putting you in the role of the pharmacy technician:
Option A: Discuss the situation with the other pharmacy technician and determine if he has an explanation as to why the OxyNEO® is not in the pharmacy stock in the safe. Since you are good friends and you have been working with him for a long time and don’t want to upset him, you tell him that if any additional issues arise you will have to bring it to the attention of the Designated Manager.
Option B: Inform the Designated Manager of the information that you have discovered and allow her to have a discussion with the other pharmacy technician. Since you feel you have done what you needed to and this is no longer your issue, you remove yourself from the situation after this point and leave any further decisions to the Designated Manager.
Option C: Although this is your friend and colleague you realize you have a professional responsibility to inform the Designated Manager of the information that you have discovered and allow her to have a discussion, with or without you, with the other pharmacy technician. You also ask that you be updated on the outcome and if unethical behaviour is identified fulfil your professional duty to ensure that the information is reported to the College and the loss to Health Canada (either by yourself or the Designated Manager).
4. IMPLEMENT AND DOCUMENT YOUR DECISION-MAKING
Select an option from the possible resolutions you identified. Ensure that you document the specifics of the information you identified and why it concerned you, including dates and details regarding subsequent conversations on the particular issue. Information like this might be required if you make any kind of report.
In this specific case, Option C is the most appropriate option. The pharmacy technician has a professional duty to look past personal conflicts of interest to ensure that the unethical behaviour is reported to the appropriate authorities. Pharmacy professionals are reminded that dual relationships, such as a friendship with a professional colleague, often place the healthcare professional’s needs whether these are emotional, financial or social in conflict with the needs, or best interests, of the patient and should be avoided.
5. REVIEW AND REFLECT
Consider the outcome of your decision and reflect on what the outcome may have been if you had chosen a different option. Review the outcome in relation to the standards in the Code of Ethics, Standards of Practice and other applicable resources and reflect on whether the outcome meets the requirements outlined in these resources. Use this opportunity to consider what you may do differently if presented with a similar situation in the future.













