Transitions of care happen when patients transfer between different care settings, such as hospital, primary care, long-term care and home care, as well as between different healthcare providers during an acute or chronic illness.[1] Due to the numerous institutions and individuals involved, as well as what can be an emotional and overwhelming time for patients and their families, transitions of care are a common time for adverse drug events to occur.
Pharmacy professionals working in all settings have a professional responsibility to support positive patient outcomes. A key component of this is understanding what both community and hospital registrants can do to provide clear and helpful information to their colleagues.
This article is part of a three-part series on transitions of care and is specifically focused on community to hospital transitions. Future articles will focus on hospital discharge as well as resources to assist in safe and quality care during transitions.
Providing Medication Lists to Hospitals
Once a patient is admitted to hospital, staff will complete a best possible medication history (BPMH) to understand what prescription medication, over the counter products and/or natural health products the patient is currently taking. To help complete this information, hospitals will often ask the patient’s community pharmacy for a list of all medications, prescription and non-prescription, on file.
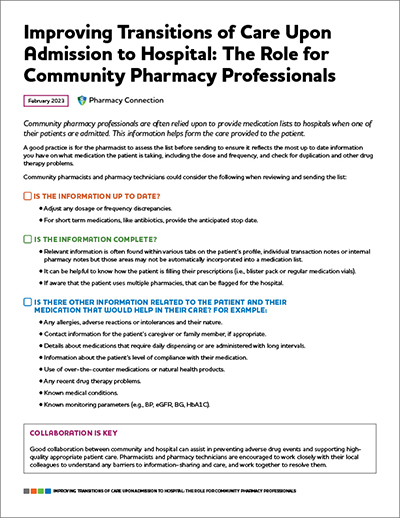
Upon request, community pharmacy professionals should provide clear and organized lists to the hospital in a timely manner. In some cases, nurses or other hospital staff may be completing the medication review and therefore may not be as familiar with the type of information provided. A good practice is for the pharmacist to assess the list before sending to ensure it reflects the most up to date information you have on what medication the patient is taking, including the dose and frequency, and check for duplication and other drug therapy problems.
Community pharmacists and pharmacy technicians could consider the following when reviewing and sending the list:
- Is the information up to date?
Ensure the current dosage and frequency is reflected.
When hospital staff or other healthcare professionals are gathering medication information for a patient, they may rely on a clinical viewer as it may be the only resource available for determining what a patient is taking if your pharmacy is closed and the patient/agent cannot provide a list. Given the importance of this information for making clinical decisions, it is critical that the information your pharmacy is submitting for publicly funded pharmacy services, ODB and NMS transactions is correct and up to date.
- Is the information complete?
Sometimes information about how a patient takes their medication is recorded in areas that would not be included on a medication list, such as comments on the patient demographic tab, notes within a transaction tab, internal pharmacy notes, or notes made in a manual format such as a blister pack binder. It can also be helpful to know how the patient is filling their prescriptions (i.e., blister pack or regular medication vials).
For example, hospital staff who are reviewing ODB prescription information from the clinical viewers for a patient on hospital admission do not see the instructions for use for the prescription. Therefore, is it important to keep the quantity of the medication accurate for the prescription so the hospital staff can try to determine how many times a patient is taking the medication in a day.
- Is there other information related to the patient and their medication that would help in their care?
There may be other information or context that a community pharmacy has related to their patient that would not appear on the list. The pharmacist may wish to consider highlighting in some way any recent changes in dosage, any medications that have been discontinued or any anticipated stop dates for use (i.e., antibiotics for a time limited period). Information about the patient’s level of compliance with their medications can be helpful in understanding what impact non-compliance or sub-therapeutic dosing may be having on their condition.
Other information could include any relevant information the pharmacy is aware of such as use of over-the-counter medications or natural health products, recent drug therapy problems, known monitoring parameters (e.g., BP, eGFR, BG, HbA1C) and known and/or recent changes in medical conditions.
It’s important to recognize that the information provided by the community pharmacy helps form the care provided to the patient at the hospital; it’s not just for knowledge or double checking. For example, orders may be generated directly from the medication list.

Pharmacist Chris Wong practices pharmacy in both community and hospital settings. He shares a few tips for community pharmacy professionals that can help support transition to hospital care for the patient.
- Include any allergies, adverse reactions or intolerances and the nature of the reaction as well as most recent height and weight, if available, with the medication list.
- Provide contact information for a patient’s caregiver, where appropriate.
- For daily dispensed medications (e.g., methadone, buprenorphine/naloxone) include when the patient last picked up the medication, and how many carries they picked up and/or the time and date of the last witnessed dose.
- For any medications that are administered with long intervals (e.g., antipsychotic injections, weekly risedronate), include the date at which patient uses, if possible. This can help avoid the patient missing any of their chronic home medications during the BPMH.
- Provide patients with a rationale and documentation when prescribing for minor ailments or prescribing Paxlovid™ to improve continuity of care if the patient is admitted to hospital. For example, if a patient was prescribed an oral antibiotic for a UTI but then it progressed to a more serious infection, it would be helpful to have a brief summary of clinically relevant interventions for a hospital physician or pharmacist inquiring about the treatment course.
- Remind patients to bring all the medications and supplements that they use to the hospital (including blister packs, puffers, creams and eye drops). If the patient has one, they should also bring an updated medication list.
Collaboration Is Key
Good collaboration between community and hospital can assist in preventing adverse drug events and supporting high-quality appropriate patient care. Pharmacists and pharmacy technicians are encouraged to work closely with their local colleagues to understand any barriers to information-sharing and care, and work together to resolve them. For example, a conversation could uncover that the local hospital system prefers a twelve-month medication history to a six month one or that there is a particular list format that better supports their system or process.
In part 2 of this article, Pharmacy Connection will focus on the transition from hospital to home, including how hospital pharmacy professionals can support their colleagues in the community. In part 3, we will focus on sharing expert resources to support transitions of care.
Sharing Personal Health Information Between Healthcare Providers
Under the Personal Health Information Protection Act (PHIPA) health information custodians, including pharmacies, can assume an individual’s implied consent to collect, use and disclose personal health information for the purposes of providing healthcare in circumstances defined in PHIPA. The ability to assume implied consent within the “circle of care” enables pharmacy professionals to exchange personal health information with other healthcare professionals in a timely manner to facilitate, and ensure continuity of, patient care.
For more information, review the College’s Releasing Personal Health Information Fact Sheet and the information and Privacy Commissioner’s of Ontario guide on Circle of Care: Sharing Personal Health Information for Health-Care Purposes.