The College has recently received several reports and complaints from patients who were given the wrong vaccine at a community pharmacy. There have been reports of mix ups between the monovalent and bivalent COVID-19 vaccines as well as mix ups between the flu vaccine and the COVID-19 vaccine. In some cases, patients received a different brand than they preferred (i.e., received a Pfizer vaccine instead of Moderna).
A foundational principle of the AIMS Program is to enable the sharing of lessons learned from medication events through reporting, which results in ongoing process improvements to minimize errors and maximize health outcomes. Encouraging a safety culture in which pharmacy professionals are comfortable having open, honest discussions about medication events within their teams without fear of punitive outcomes, makes pharmacy and the collective health care system safer.
De-identified, aggregate data from the AIMS Program shows that, since the initiation of the COVID vaccination program, there have been 754 events recorded related to COVID-19 vaccines, with 96% of them being incidents, meaning they reached the patient. While the harm level was generally classified within AIMS as none or low, incidents such as these can erode public confidence in the care that they receive from the pharmacy. In addition, if the error is not caught, a patient could believe they have some level of protection that they didn’t receive (i.e., they think they’ve received their COVID vaccine and have that protection, but instead got a second flu shot.)
The most common contributing factors for incidents reported through AIMS were staffing issues, lack of staff education, drug-related issues such as look-alike packaging and unclear or absent labelling, missing patient information, lack of quality control systems and miscommunication of drug orders.
Addressing Contributing Factors in Workflow
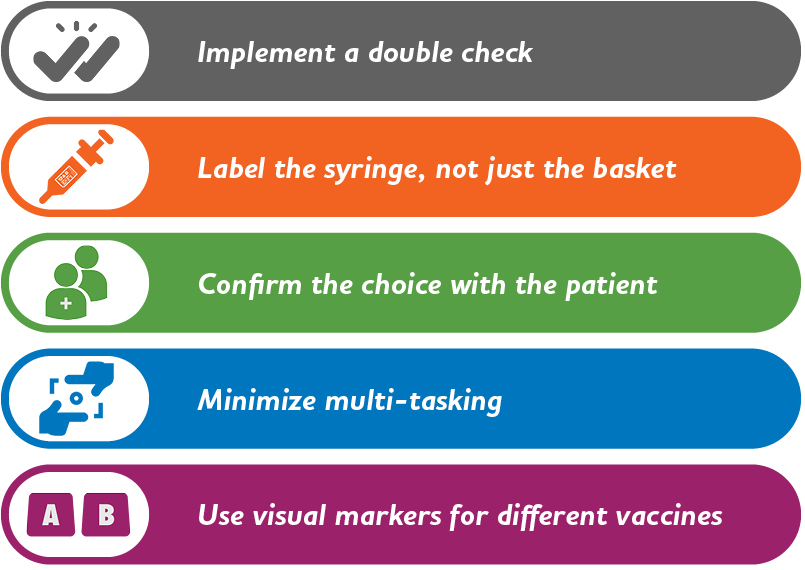
Preventing these types of incidents can involve changes to workflow at the pharmacy. Based on the aggregate and de-identified contributing factors data from AIMS, here are some potential practices to consider:
- Implementing a double check system. Consider whether there is a way to incorporate a double check into the pharmacy’s workflow. For example, a second pharmacy professional could check and sign off on the vaccine that was used to prepare syringes.
- Using labels on the syringes in addition to the basket. Even if prepared doses are sorted into labelled baskets, it is a good practice to place labels directly on each syringe as well. This can help prevent confusion if a syringe ends up separated from the basket.
- Confirming with the patient their choice prior to administration. For example, asking the patient, with an open-ended question, which vaccine they want to receive immediately prior to administering the injection. Pharmacy professionals can also give the patient an opportunity to view the label of the syringe to confirm for themselves.
- Minimizing multi-tasking between immunizations and patient care activities as much as possible. Moving quickly between preparing medications, speaking with patients, managing administrative tasks, and administering injections can increase the likelihood of an error. If the pharmacy is providing a significant number of vaccinations, the Designated Manager can consider assigning a staff member to primarily administer injections for a particular period of time (e.g., between 1 and 3 pm or only on certain days of the week) or to offer vaccines by appointment only to allow for an uninterrupted workflow. A well thought out workflow for preparing and administering vaccines can also assist with minimizing multi-tasking.
- Separating monovalent COVID vaccines from bivalent vaccines. The vials for certain monovalent and bivalent vaccines can look very similar. To help distinguish the distinct versions of vaccines, multiple visual markers can be used, including storing on a different shelf in the fridge, posting warning signs to double check the type, or using a different colour of basket or container for each version.
Looking at Your Pharmacy’s Workflow: Practices to Help Prevent Vaccine Errors
Vaccine Scheduling Resources
Pharmacy professionals who have questions about the scheduling of COVID vaccines and boosters, should consult the Ministry’s COVID-19 Vaccine Guidance document.













