As a regulator increasingly focused on health system and patient outcomes, the College is committed to working with stakeholders to enable a collaborative approach to healthcare. The College recognizes the important role that pharmacy professionals play in the broader healthcare system, and has embedded a systems-focus in many of its key initiatives, including Quality Indicators, AIMS and the work to enable expanded scope of practice for pharmacists.
OCP recently partnered with Ontario Health (North) and Ontario Health (Quality) to develop a systems approach to enable collaboration between primary care and community pharmacy to improve care for patients with depression.
In northern regions there are unique challenges which serve as barriers to treating patients with mental health disorders. These include low health care provider-to-population ratios, travel time to reach service providers, local demand for services, and percentage of repeat hospital stays for patients with mental illness. Strengthening the integration of primary care and community pharmacy will help to provide care across the continuum and better support patients with depression.
This project aimed to develop and test a model demonstrating the benefits of provider collaboration in delivering care for patients in two northern communities (Sudbury and Espanola). This model, aligned to the Ontario Health (OH) Quality Standard for Major Depression, involves primary care practitioners asking patients to connect with their community pharmacist who provided regular follow-up and monitoring as well as additional supports regarding adjunct therapies for self-management.
A shared model assists professionals to contribute in a meaningful way to patients and the system by providing the right level of support in an accessible location to achieve healthcare goals and, in some cases, improve access to care.
The role of the College was to help the project partners navigate regulatory responsibilities of pharmacy professionals in designing and implementing the model and to demonstrate support for pharmacies to participate in these types of quality improvement approaches in their own communities.
FOCUSING ON THE FIRST SIX WEEKS OF CARE
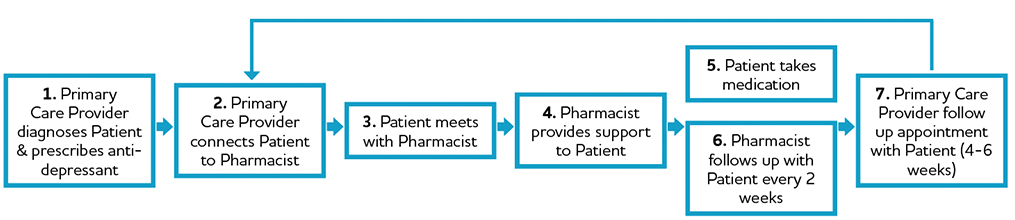
In this model, the pharmacist would meet with the patient, after receiving a prescription from the primary care provider, to assess their health status, discuss their health and well-being, and provide appropriate education on their prescription as well as any additional recommendations regarding their health (i.e. services in their local community, non-medication supports). The pharmacist follows up with the patient at two weeks and four weeks after dispensing to assess their health status, discuss their adherence and response to the medication and offer support in terms of suggesting adjunct therapies or community resources. Throughout this process, the pharmacist is encouraged to communicate with the primary care provider as needed (i.e. updates on the patient health status, recommendations for changes to medication, additional supports provided). Pharmacists were provided with a toolkit of resources to guide their discussions with patients.
RESULTS FOR PATIENTS, PROFESSIONALS AND THE DEVELOPMENT OF FUTURE MODELS
Throughout and after implementation of the model, patients, primary care providers and pharmacists were asked to contribute to measurement and evaluation. The majority of patients felt that the additional supports were helpful and would recommend them to friends and family. Participating healthcare professionals found that the collaboration between primary care providers and pharmacists was helpful to patients. Overall, it was demonstrated that there was value in working in this sort of collaborative quality improvement model to support good outcomes for patients.
Key enablers of the success of the model included establishing new relationships and engaging upfront with primary care providers, adapting staffing at the pharmacy to allow pharmacists to take on this role, and facilitating access to health records, such as through the ClinicalViewer.
As a next step, the toolkit will be shared to enable others to adapt the model to their practice. It is anticipated that this process, whereby community pharmacies and primary care collaborate to implement Ontario Health Quality Standards, could be adapted to other conditions such as COPD and diabetes. It could also be applicable to Ontario Health Teams, where community pharmacists can play a role in a team-based model of care.
WORKING TOGETHER TO SUPPORT PATIENTS:
One Pharmacist’s Experience with the Community Pharmacy and Primary Care Model
Lynn Halliday is a pharmacist at Espanola Clinic Pharmacy who participated in the project. Below, she shares her experience as well as advice for pharmacists who may want to integrate a similar quality improvement approach in their pharmacies.
How did you engage with primary care providers as part of this project? And what advice would you have for pharmacists who want to build more collaborative relationships with primary care providers in their community?
Since our pharmacy is in the same space as the physician offices, I mostly “marched” back to talk with our physicians in person whenever issues arose. Initially the head of the Family Health Team hosted a meeting with all of the physicians to explain the project and I was allowed to present the pharmacy perspective of this project. This was terrific because I was able to get first hand input from them and to discuss what they wanted feedback on and how they wanted to receive it. There was some questioning at this meeting about the need for pharmacists in the project and this gave me a terrific opportunity to present the case for collaboration with pharmacy.
My advice for other pharmacists is to make opportunities to speak directly with their main physicians about how best to communicate with them, whether via email, fax, memos or phone calls then try your best to keep the information short, to the point and given in the manner that they wish to receive it.
What were some of the benefits you saw for your patients as a result of this approach?
My patients felt that they were cared for, because I would call them. They were usually glad to receive these calls especially since their condition often made them feel neglected, sad and alone. Establishing relationships is so important to people. In addition, the longer the patient took their medication properly, the better they felt. When they had problems due to the medications, I was there to help them to problem solve the issues, thereby keeping them on their medication when they otherwise would have stopped.
What was the time commitment to participate and how did you integrate it into your workflow?
This required very little extra time, since counselling on new prescriptions is standard and I follow up with many new prescriptions anyway and already have a process in place. For the timeframe of the actual project I had to record the patients enrolled and activities on a spread sheet, this was a matter of five minutes per day.
I think that each pharmacist can do follow ups by learning to use the pharmacy management system to alert and record. I used my system (we have Kroll) to document both my follow up appointments and responses to these calls. Then I used my standard Professional Opinion form to inform physicians of any issues or adaptations that occurred as a result of the calls. Using the Professional function in Kroll, I was able to record the initial interview with my patient and schedule a follow up. Once I completed the follow up call or visit, I then used the follow up tab to record pertinent details, which then recorded to the original interview note with a new date. Learning how to use this function was an important “take-away” that I have now applied to other medication documentation.
Being organized is the key. Making follow up phone calls can be a bit time consuming, but with organization it can be done in the slow moments, during regular flow. I try to print the list of follow up calls for the day at the beginning of my shift, then I work my way through the list when I get quiet dispensing moments. I save the calls to students and working patients for nights and weekends.
Did you identify any other key learnings or changes to your practice as a result of taking part in this project?
It’s important to have the right resources in one place to help patients cope with this illness and support discussions with them. For example, a community “help” chart with contact or program names that I can recommend to patients who need support.
Even though this project has ended, I will informally continue to do follow ups with this group of patients and also with others as needed.
This design could be adapted to many different diseases and can fit into the normal flow of the pharmacy. The partnership of the primary care provider and the pharmacist allows the provider to initiate therapy and the pharmacist to help keep it going.
ACCESS PATIENT INFORMATION THROUGH CLINICAL VIEWERS IN ORDER TO SUPPORT BETTER PATIENT CARE
Pharmacies are able to access provincial patient information through secure, web-based clinical viewers hosted by Ontario Health (either ConnectingOntario ClinicalViewer or ClinicalConnect.)
Patient information provided through the clinical viewers includes:
- Medication information (publicly funded dispensed drugs, dispensed monitored drugs, pharmacy services)
- Laboratory results (from the Ontario Laboratories Information System)
- Discharge summaries (from the Acute and Community Care Clinical Data Repository)
The dynamic view of patients’ health information provided by the clinical viewer can both support the work of pharmacy professionals in delivering counselling, support and treatment, and contribute to better patient care.
There is no cost to pharmacies to participate. To sign up for access to the clinical viewer, the pharmacy’s Director Liaison or Designated Manager must complete a request to “Onboard My Organization” on the Ontario Health website for either ConnectingOntario Clinical Viewer or ClinicalConnect.













