Samantha Li,
RPh, BSc, MSc, PharmD1
Larry Sheng,
BSc, PharmD Student2
Certina Ho,
RPh, BScPhm, MISt, MEd, PhD1,2,3
1Leslie Dan Faculty of Pharmacy, University of Toronto
2School of Pharmacy, University of Waterloo
3Institute for Safe Medication Practices Canada
As patient cases become more complex, it is inevitable that more healthcare professionals will be involved in their circle of care (1). These healthcare professionals may include family physicians, specialists, nurses, and pharmacists. As such, it is crucial that all healthcare providers in the circle of care effectively communicate with their team mates, have a clear understanding of the care plan, and collaborate to provide optimal patient-centered care (1). However, in reality, healthcare providers may be unaware of their team mates’involvement and this may contribute to minimal inter-professional communication, and a lack of complete awareness surrounding details of the patient’s intended care plan. This is particularly challenging in outpatient/ambulatory care and community pharmacy settings where healthcare professionals may be distributed in different geographical regions. Communication gaps between patients and among different healthcare providers can have negative impacts on patient care and, more importantly, on patient outcome and safety (1-3).
The Institute for Safe Medication Practices Canada (ISMP Canada) Community Pharmacy Incident Reporting (CPhIR) program (http://www.cphir.ca) was used to generate a list of medication incidents (anonymously reported by community pharmacies) that were associated with moderate to severe patient harm from 2009 to 2017. A total of 134 medication incidents were included for a qualitative multi-incident analysis conducted by two ISMP Canada medication safety analysts. Themes, sub-themes, and contributing factors of the medication incidents were identified, and recommendations were derived to address safety gaps in patient care (Table 1).
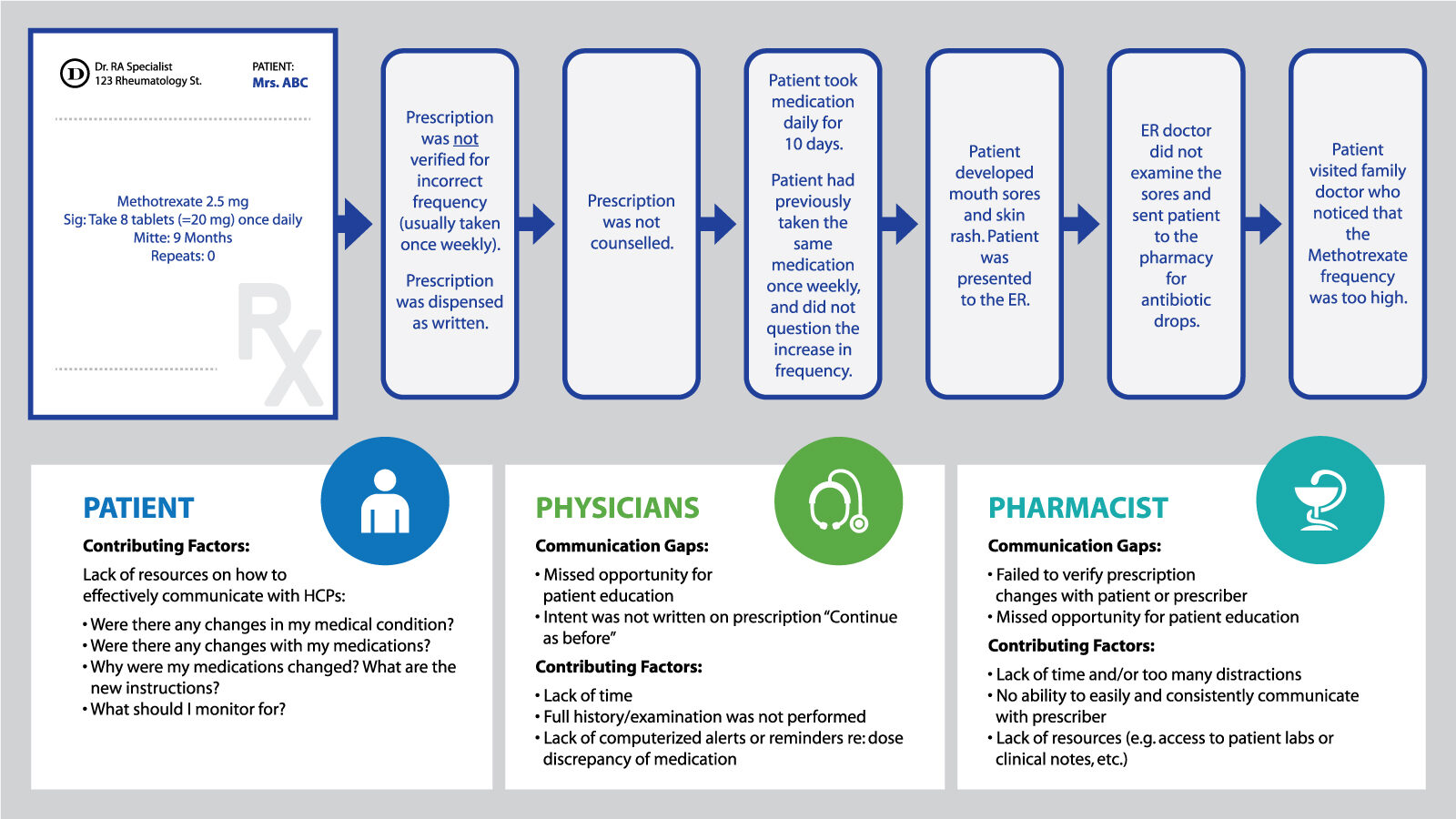
From the 134 medication incidents that were identified, 78 involved communication gaps of which three main themes were identified: (1) Gaps in written communication; (2) Gaps in verbal communication; and 3) Lack of communication. We further derived sub-themes from these main themes: (a) Gaps in communication between healthcare providers; and (b) Gaps in communication between healthcare providers and patient. Selected examples of medication incidents that involved various degrees of communication gaps are provided in Table 1 and Figure 1.
We identified the following common contributing factors of medication incidents that involved communication gaps (Table 1): (1) lack of a standardized information gathering process or technique; (2) hectic work environment with time constraints; (3) ambiguous prescription instructions; (4) look-alike/sound-alike drug names; and (5) confirmation bias.
| Communication Gaps | Incident Example | Contributing Factors |
|---|---|---|
| Written Communication Gap | Refer to Figure 1 | Refer to Figure 1 |
| Verbal Communication Gap | Patient has prescriptions for Warfarin 1 mg and Warfarin 5 mg on file at the pharmacy. Patient called and asked for a refill for Warfarin but no strength was indicated. Pharmacy assistant refilled for Warfarin 5 mg. Patient took Warfarin 5 mg, as opposed to Warfarin 1 mg, which he had intended to refill. Patient’s INR was not controlled. |
|
| Lack of Communication | Patient has an allergy to Amoxicillin. Neither patient nor pharmacy team discussed allergies during prescription drop-off. Patient picked up Amoxicillin prescription and declined counselling. Patient took medication and experienced an anaphylactic reaction. |
|
Table 1. Communication Gaps in Pharmacy Practice
Figure 1. An example of a medication incident that involved communication gaps: (a) Gaps in communication between healthcare providers; and (b) Gaps in communication between healthcare providers and patient
COLLABORATION BETWEEN PATIENTS AND HEALTHCARE PROVIDERS
An essential competency for healthcare professionals is effective communication skills (4, 5). In order to address communication gaps, patients and their healthcare providers need to recognize the challenges and effectively communicate amongst themselves.
Healthcare professionals must develop an information gathering process that is standardized, efficient, and comprehensive. In addition, they must engage in open dialogue with their patients as it is important to build a strong rapport with them (4). Decreasing the interaction or time with patients may negatively affect the ability for patients and healthcare professionals to build a trusting relationship and, more importantly, it may impact patient/medication safety.
Technology has enabled instantaneous communication with anyone, anywhere, at any time. However, as people communicate more frequently, the form of content becomes increasingly superficial and ineffective (6, 7). This trend is apparent in the digital world but it is also influencing interpersonal communication skills (6, 7). Moreover, some patients may be pre-occupied with their mobile devices when picking up prescriptions. This may distract them from receiving and understanding critical patient counselling points in their medication therapy management and compromise the overall quality of care and patient safety.
Information Gaps
Lack of information is usually a two-fold problem: (1) pharmacists may not have enough information to safely dispense a medication; and/or (2) patients are not knowledgeable or not fully informed about their medical condition(s) and intended care plan; and they are not aware of the questions they should ask about their medications, etc.
Patients are the common denominator that connects all members of the circle of care. As such, patients should be seeking necessary information from their healthcare providers, such as changes in their medication(s), the nature/rationale of medication therapy adjustments, and what actions or monitoring parameters are required on their part as patients (8-10). Although patients may expect that all healthcare providers in their circle of care are communicating with each other regarding their care plan, unfortunately, this may not always be the case (1, 3, 11). Information exchange among healthcare practitioners is often perceived to be incomplete (11). Furthermore, it is also possible that some healthcare providers, depending on their practice settings, do not have access to critical information (e.g. lab values and diagnostic test results) that is required to support decision-making for optimal patient care (12). A common example is that community pharmacists often play broken telephone trying to piece information together from various resources: prescriptions or medication records, patient profile, and contacting the prescriber, if necessary, etc. in order to safely dispense a medication within time constraints (12). This practice is not only time-consuming but may also put patients at risk of medication harm, especially if wrong assumptions or confirmation bias are made during the medication-use process.
Educating Patients
Healthcare practitioners need to educate their patients on what to ask and document during each patient encounter. This begins with a clear communication strategy. The American College of Clinical Pharmacy suggests using simple non-medical language, limiting the amount of content, using visual aids, increasing patient participation, and emphasizing key counselling points as techniques for clear communication (13). Furthermore, there are several Canadian resources that can support patients with effective communication. This includes HealthLinkBC’s printable patient reference sheets (available from https://www.healthlinkbc.ca/health-topics/hw226888), a resource that encourages patients to ask important questions during different medical appointments (for example, new ailment diagnosis and follow-up appointments) (9).
Before the patient leaves the clinic, healthcare practitioners should ensure their patients have a basic comprehension of their care plan. Counselling techniques such as show and tell and teach back can help healthcare professionals gauge patient’s understanding (2). In addition, the Institute for Safe Medication Practices Canada (ISMP Canada), the Canadian Patient Safety Institute, Patients for Patient Safety Canada, the Canadian Pharmacists Association, and the Canadian Society for Hospital Pharmacists have collaborated and developed the 5 Questions to Ask About Your Medications (available from https://www.ismp-canada.org/medrec/5questions.htm) to help patients initiate a dialogue with their healthcare providers about their medications. Effective and efficient communication becomes second nature when both parties come prepared for the encounter.
Educate your team
A community pharmacy team often consists of pharmacists, technicians, and assistants. Very often, technicians and assistants have the first interaction with patients via an in-person encounter or a phone conversation. Therefore, all members of the pharmacy team should be educated and informed on the importance of communication and comprehensive information gathering techniques. This would optimize work flow and improve patient safety.
Use technology
Current communication techniques, such as fax and telephone, are inefficient and may overload the workflow or practice setting with paper. In the near future, the healthcare system will require better tools or strategy to facilitate seamless communication among healthcare professionals and help prioritize tasks with respect to the increasing demands of patient-centered care. A fully functional e-health system where healthcare providers have ready access to a patient’s complete medical and medication records will become the gold standard. Meanwhile, healthcare practitioners should better utilize and demand more from their point-of-care clinical decision support applications that may allow or support safety features, such as reminders for updating patient medication lists and alerts for dose discrepancy (e.g. dose too high, or dose too low). These are some examples of how current technology may help healthcare providers deliver safe and effective patient care.
OVERCOMING BARRIERS AND OPTIMIZING COMMUNICATION TECHNIQUES
Poor communication degrades the quality of patient care. Barriers to effective communication include logistical factors, such as healthcare providers being unaware of other healthcare providers within a patient’s circle of care and relying on ineffective means of communication for information transfer/exchange (e.g. fax and telephone). Leveraging current technology and informatics could combat such challenges. Optimizing communication techniques (e.g. computerized physician order entry (CPOE) or electronic pre-printed prescription orders), standardizing information-gathering strategies (e.g. adopting a consistent process to conduct a Best Possible Medication History (BPMH) (available from https://www.ismp-canada.org/download/MedRec/SHN_medcard_09_EN.pdf)), and facilitating effective workflow should be ongoing safety initiatives in any healthcare setting. Ultimately, everyone who is involved in a patient’s care (including the patient) should be responsible for effective and efficient communication. Failing this responsibility often translates to delays in patient care and/or risks to patient health and safety.
REFERENCES
- Vermeir P, Vandijck D, Degroote S, Peleman R, Verhaeghe R, Mortier E, et al. Communication in healthcare: a narrative review of the literature and practical recommendations. International Journal of Clinical Practice 2015;69(11):1257-67.
- Boucher A, Dhanjal S, Kong JH, Ho C. Medication incidents associated with patient harm in community pharmacy: A multi-incident analysis. Pharmacy Connection 2018;Winter:38-42.
- Shitu Z, Hassan I, Aung M, Kamaruzaman T, Musa R. Avoiding medication errors through effective communication in a healthcare environment. Malaysian Journal of Movement, Health, & Exercise 2018;7(1):115-28.
- ACOG Committee Opinion No. 587: Effective patient-physician communication. Obstetrics and gynecology 2014;123(2 Pt 1):389-393.
- Association of Faculties of Pharmacy of Canada (AFPC). Position Statement and Joint Resolution on the Doctor of Pharmacy (PharmD) for the First Professional Degree at Universities in Canada – February 2010. Available from http://www.afpc.info/node/37
- Turkle S. The flight From conversation. The New York Times 2012; April 21: Sunday Review (Opinion). Available from: https://www.nytimes.com/2012/04/22/opinion/sunday/the-flight-from-conversation.html
- Turkle S. Stop googling. Let’s talk. The New York Times 2015; September 26: Sunday Review (Opinion). Available from: https://www.nytimes.com/2015/09/27/opinion/sunday/stop-googling-lets-talk.html
- He T, Ho C. Patients as the last slice of swiss cheese. Hospital News 2017; April: 38-39. Available from: https://www.ismp-canada.org/download/hnews/201704-HospitalNews-SwissCheese.pdf
- HealthLinkBC. Making the most of your appointment. 2017 October 9. Available from: https://www.healthlinkbc.ca/health-topics/hw226888
- Nguyen C, Ho C. Five questions to ask about your medications. Hospital News 2017; February: 18. Available from: https://www.ismp-canada.org/download/hnews/201702-HospitalNews-5Questions.pdf
- Gandhi TK, Sittig DF, Franklin M, Sussman AJ, Fairchild DG, Bates DW. Communication breakdown in the outpatient referral process. Journal of General Internal Medicine 2000;15(9):626-631.
- Chen YF, Neil KE, Avery AJ, Dewey ME, Johnson C. Prescribing errors and other problems reported by community pharmacists. Therapeutics and Clinical Risk Management 2005;1(4):333-342.
- McConaha JL, Prosser TR. Communication strategies in pharmacy. ACCP Updates in Therapeutics® 2017: Ambulatory Care Pharmacy Preparatory Review and Recertification Course. Available from: https://www.accp.com/docs/meetings/UT17/handouts/02._Communication_Strategies_in_Pharmacy.pdf