The College’s practice advisors regularly assess pharmacists and pharmacy technicians in their place of practice. During practice assessments, advisors have noted some common areas where registrants are not meeting the expectations of the Standards of Practice. Here are five practice essentials to support safe and quality patient care:
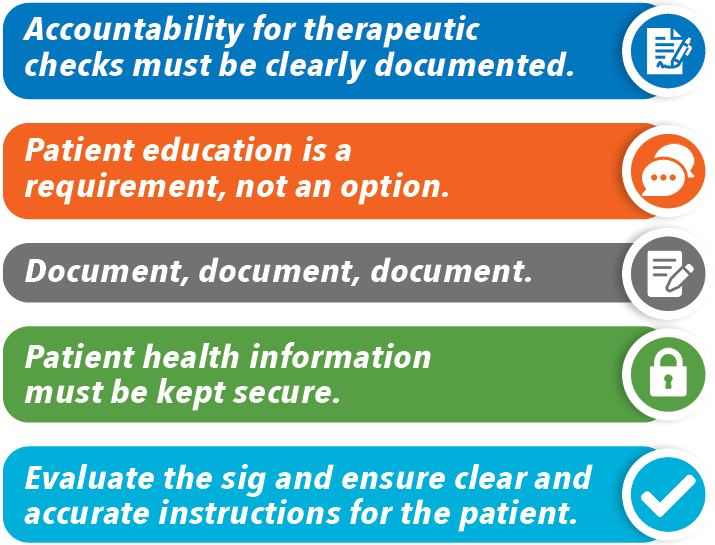
1. Accountability for therapeutic checks must be clearly documented
A therapeutic check by a pharmacist is required before releasing medication to a patient. A pharmacy technician cannot perform the technical check and release the prescription, even if it’s a refill, unless the therapeutic check has been completed.
It should always be clear who is responsible for the therapeutic check of a prescription. If there are multiple pharmacists working within the pharmacy, there should be an established process in place to indicate who was responsible for the therapeutic check, such as using a protected credential or unique identifier (e.g., initials, manual signature, digital signature).
Resources
- Ensuring Therapeutic Appropriateness for New and Refill Prescriptions (Pharmacy Connection)
2. Patient education is a requirement, not an option
Pharmacists must provide information and educate patients about their medication to enable the patient to receive the intended benefit. These conversations help pharmacists gain insight into patient understanding, which is important for confirming that patients are taking their medications appropriately, and assist in obtaining all the information needed about that patient and the prescription to make a proper therapeutic assessment. Check-ins with the patient also contribute to identifying any red flags and support ongoing follow-up and monitoring.
In their assessments, College advisors have observed many incidents of declined counselling. Pharmacy staff should not suggest to patients that education (counselling) may not be necessary or override the requirement; the pharmacist must make the decision, ideally in consultation with the patient, regarding whether education is required.
When pharmacy staff “decline” an opportunity for education, it also removes the final chance to identify a medication incident before the medication leaves the pharmacy. Ultimately, it is the responsibility of the pharmacist to decide if it is appropriate to release the prescription.

Resources
- Interactive Approach is Effective in Fostering Patient Dialogue and Education (Pharmacy Connection)
- Promoting Safety Through Conversation: Patient Assessments (Pharmacy Connection)
3. Document, document, document
If you didn’t document it, it didn’t happen. Information gathered during the patient assessment, patient education provided, decisions made and their rationale, necessary follow-up and any other relevant information should be documented as soon as possible. Relying on memory or postponing documentation to another time can increase the risk of error. Relevant information should be captured in a focused and concise manner that makes sense for your pharmacy’s workflow and software system.
Factual, complete, up to date, and organized documentation supports continuity of care by all members of the pharmacy team. Additionally, if questions or concerns are later raised regarding the patient’s care, documentation can confirm the actions taken.
Resources
- Documentation: Essential to a Patient’s Continuity of Care (Pharmacy Connection)
- The Four R’s of Documentation (Pharmacy Connection)
4. Patient health information must be kept secure
When following up with patients for monitoring purposes (e.g., minor ailments prescribing, medication adjustments), it’s important to ensure that patient information is not being shared or exchanged on unsecured channels.
For example, voicemails may be accessible to multiple household members, so consider only asking the patient to call the pharmacy rather than leaving detailed information about medication, medical conditions or other confidential information.
When communicating electronically with patients or other healthcare providers, registrants are strongly recommended to use encrypted communication and/or secured healthcare-specific software and applications to communicate personal health information to prevent privacy breaches. Unencrypted messaging, such as unsecured texting, email or other messaging applications, presents numerous risks, including the interception of messages, issues with retaining and retrieving information, loss or theft of mobile devices, and use of unsecure networks.
If only unencrypted messaging to patients is available, registrants should avoid including personal health information (i.e., only communicating regarding administrative matters such as scheduling or reminders). Additionally, express consent should be obtained from the patient (and documented) before sending any personal health information.
Resources
5. Evaluate the sig and ensure clear and accurate instructions for the patient
When completing technical checks of a prescription, it is important to evaluate the sig (directions for use from the prescriber). Instructions should be clear to/for the patient, accurate and use appropriate punctuation.
Directions on a prescription label should match how a patient is intended to use the medication. Verbally providing instructions that are different from the directions on the label can be confusing to patients and lead to medication errors. If the directions on the label are unclear or could be misinterpreted, pharmacists should utilize their scope to address this (i.e., consideration can be given to adapting the prescription or contacting the prescriber).
For example, the use of “as directed” can lead to misunderstandings about how and when to take a medication, including preventing pharmacists from effectively educating patients (e.g., pharmacists might not know what the prescriber told the patient) and patients from taking their medication correctly (e.g., patients don’t remember what they were told).[1]
Correct and clear instructions allow information to be conveyed accurately to the patient and minimizes the opportunity for errors in how the medication is used. It also helps to maintain clear records for the pharmacy, which is crucial in the event information must be transmitted/transferred to other health care providers (e.g., if a patient is admitted to the hospital).
Resources
Registrants can change their DPA site at any time through their online profile. This information must be up to date as the College and practice advisors depend on the accuracy of this information to schedule and attend the practice assessment.
- Grissinger M. “Use as Directed” Can Cause Confusion for Both Patients and Practitioners. P T. 2019 Apr;44(4):168-169. PMID: 30930599; PMCID: PMC6428496. Accessed: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6428496/ ↑













