Part 1 of this series on transitions of care, Improving Transitions of Care Upon Admission to Hospital: The Role for Community Pharmacy Professionals was published in March 2023 and focused on how community pharmacy professionals can support quality care when their patient is admitted to hospital. In this Part 2, we will focus on how to support the transition home. In Part 3, we will highlight resources to assist in safe and quality care during transitions.
Team-Based Effort
All healthcare professionals have a responsibility to work collaboratively to support safe and effective patient care. Transitioning between various healthcare settings, all with their own processes, staff, and records management systems, is a time when patients are most at risk for an adverse drug event.
Given that there is no standardized system, every hospital will have their own mechanisms and software for discharging patients to the community, including the templates used for documentation and prescriptions. It’s also important to recognize that many healthcare professionals involved in hospital discharges are not pharmacy professionals but rather physicians, nurses and clerks.
Ongoing collaboration between hospitals and community settings can support system improvements. Regular communication on the issues experienced during transitions of care can help identify process improvements. One example might be setting up recurring meetings between local hospitals, a representative of a local community pharmacy group and local patient/advocate groups, if there is one, to discuss challenges. There may be other health system partners to include as well, such as local Ontario Health Teams or family physician groups.



Providing Community Pharmacy Professionals with Essential Information During Discharge
Though pharmacy professionals working in hospitals may not have ownership over the discharge process, there may still be opportunities to influence how their organization approaches patient discharges.
In doing so, key considerations can include:

Focusing on the key information that community pharmacies will need and providing it in a clear and organized structure. In most cases, this information will include what medications have been started/added for the patient, what medication they continued to take, what medication they stopped while in hospital, as well as any changes in dose or frequency.
Ideally, information would also be provided on the indication for each medication and/or change in dose (for example, a change in renal function). In addition, information about any OTCs, vitamins and natural health products should be included. Consider including information that a community pharmacist may require to support dispensing such as limited use codes and the need for blister packaging.
Prescribers, pharmacy professionals and others involved in the discharge process should also be aware of prepopulated comments that may be added automatically as part of the medication administration record. If not appropriate to the intended use of the medication or not adapted to the specific needs of the patient, these comments could cause confusion for the community pharmacy and patient.

Understanding the information that community pharmacies may or may not have access to. Many community pharmacies do not have access to Clinical Viewers to see lab work or hospital discharge information and so it may make sense to include information related to the reason for the hospital visit and any necessary follow-up on the discharge paperwork. (Community pharmacies are strongly encouraged to sign up for Clinical Viewers.)

Recognizing the impact of cost and availability. Though it may not be possible with the current resource challenges in healthcare, a best practice would be to contact a patient’s community pharmacy in preparation for discharge to understand whether the medication for the patient is covered under their drug program or insurance and whether it is even available.
It’s important to be aware that the hospital formulation may be different than what is covered by public drug program. Providing generic names instead of only brand names can be helpful.
Concerns about affording or accessing medications can be an additional stress on patients and families, cause unnecessary back and forth between pharmacy and prescriber and may even be a risk factor for readmission if the patient cannot access their medication in a timely manner.

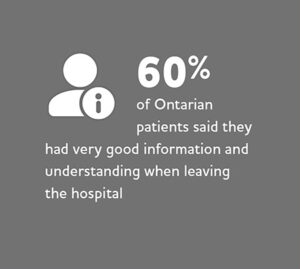
Involving the patient. In discussions held with the patient and/or caregiver prior to discharge, hospital staff may wish to emphasize with them what information is critical to share with the community pharmacy, that they should take all hospital discharge papers to the pharmacy, and the importance of having one consistent pharmacy to prevent issues with continuity of care. For example, patients should know why they are on each medication, why there have been any changes to their medication or dose, and what they should be taking upon discharge[1].
Having these conversations well in advance of the discharge time can allow for appropriate planning, such as allowing prescriptions to be sent to the preferred community pharmacy ahead of time or arranging for necessary translation or support.
Tips from a Pharmacist

Lisa MacEachern is a community pharmacist and chair of the Guelph Pharmacists Association who has collaborated with local hospitals on their discharge processes. Here she shares some learnings for hospitals and community pharmacies:
- Hospitals should make sure it is clear how to contact the hospital inpatient pharmacy, and any specifics regarding that process such as hours of operation, on the discharge information in case of any questions from the community pharmacy.
- Community pharmacists should contact the hospital inpatient pharmacy directly with any questions about what the patient was taking in hospital, as the pharmacy will likely be able to access this information easier than the nurse or physician.
- Hospital pharmacy staff can contact the patient’s community pharmacy before discharge to ask if a medication the patient has been taking in hospital is available or covered for the patient and/or to flag any significant medication changes that will require additional attention of follow-up.
- It is a good practice for hospitals to keep their discharge forms clear by not listing all medications in one list, but instead having separate sections on the form to include home medication for the patient, stopped medication, medications on hold until the physician can assess the patient, and what medications should be continued.
- Hospitals are encouraged to provide a place to document important notes from the prescriber at the top of the discharge form or in another place where they won’t be missed. Notes should be clear so that they can easily be inputted by any pharmacy staff into the computer system.
- Hospital discharge information, and any changes to medication as a result, should be shared with the patient’s primary care provider.
- It is helpful to have a liaison between community pharmacy and hospitals to discuss transitions of care and how both processes can be changed to help.
- Community pharmacy professionals should look for opportunities to develop good working relationships with hospital registrants within their community.
The access and release of patient information following discharge from the hospital may be governed by specific policies or procedures at the hospital. Pharmacy professionals should work with their institution’s privacy officer to understand any requirements.
In general, pharmacists and pharmacy technicians, as health information custodians under the Personal Health Information Protection Act (PHIPA), can assume an individual’s implied consent to collect, use and disclose personal health information for the purposes of providing healthcare in circumstances defined in PHIPA. The ability to assume implied consent within the “circle of care” enables pharmacy professionals to exchange personal health information with other healthcare professionals in a timely manner to facilitate, and ensure continuity of, patient care.
For more information, review the College’s Releasing Personal Health Information Fact Sheet and the information and Privacy Commissioner’s of Ontario guide on Circle of Care: Sharing Personal Health Information for Health-Care Purposes.
Special thanks to Hina Marsonia for reviewing this article.
- ↑ Discharge Medication Management Toolkit. Canadian Society of Hospital Pharmacists. https://www.cshp.ca/docs/pdfs/Discharge-Medication-Management-Toolkit-Sep%2023.pdf













